Cancer Prevention and Treatment
Identifying Gene Abnormalities can empower the early treatment and prevention of cancer
Genetic testing can detect the signs of cancer at an early stage, enabling the prevention and treatment of disease even before tumors are formed
Conventional cancer treatments fall into three key modalities—surgery, chemotherapy, and radiotherapy. In each of these treatment modalities, therapeutic measures are applied from outside the body. HIC Clinic’s gene therapy, however, is administered via intravenous infusion to repair the genetic damage of cancer from inside the cell. Based on your symptoms and disease stage, we recommend the concomitant use of multiple treatment modalities for optimal outcomes.

Cancer Prevention and Treatment Services Offered by HIC Clinic
Tumor-Suppressor Gene Therapy
This form of therapy serves both to prevent cancer and to treat cancer by controlling the tumor suppressor genes that regulate oncogene functionality. There are many different tumor suppressor genes including P53, P16, TRAIL, and PTEN; and our genetic tests have the ability to identify which of these may be abnormal in your DNA. Once these abnormalities are identified, we are able to administer gene therapy tailored to suit your specific genetic profile.
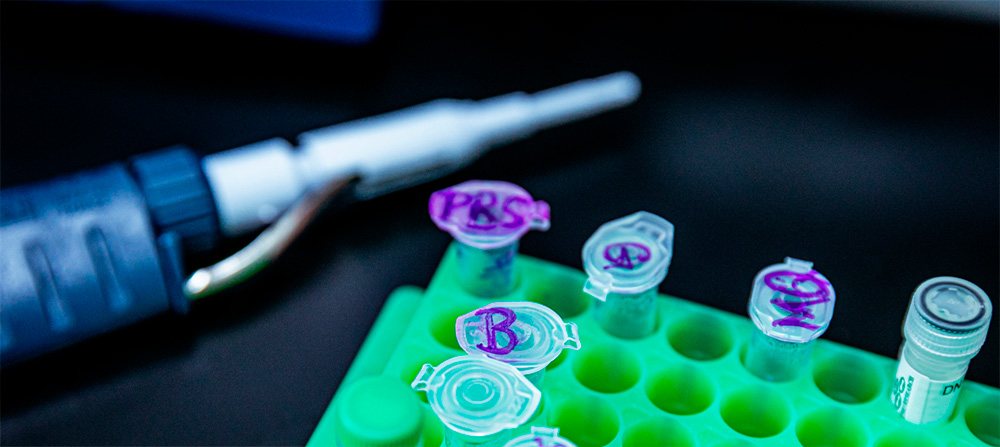
Because each and every individual has a different pattern of genetic mutation, HIC Clinic runs assays to identify 251 different genetic aberrations. As a result, each patient is provided a personalized plan for cancer prevention or treatment that is tailored to their specific needs.
For cancer prevention, our Tumor-Suppressor Gene Therapy is effective on its own. This monotherapy is also beneficial for individuals with approximately two to three genetic abnormalities.
For people with more genetic defects, we recommend a combination regimen, in which our gene therapy is combined with DNA vaccines and/or a variety of cell-based therapies.
When patients have an established cancer diagnosis, we repair their genetic abnormalities using our gene therapy before administering conventional therapies such as chemotherapy and/or radiotherapy. We find that in many cases this sequential approach results in more favorable outcomes.
Such an approach can provide additive clinical benefits. For example, chemotherapies are often ineffective in patients carrying methylated or mutated tumor suppressor genes. However, the prior administration of our gene therapy can serve to activate the function of tumor suppressor genes to improve the efficacy of subsequent chemotherapy.
In some malignancies, the success of radiotherapy may depend on the functionality of the P53 tumor suppressor gene. So in a manner similar to that with chemotherapy, the prior administration of our gene therapy may serve to upregulate P53 expression, resulting in improved patient outcomes with subsequent radiotherapy.
DNA Vaccines
DNA vaccines are essential for mounting an effective immune response against cancer
HIC Clinic’s DNA vaccine therapies work by injecting specific DNA fragments into the body that cause immune cells to produce cancer-specific proteins or antigens. These proteins and antigens, in turn, elicit an immune response directed at cancer cells with that specific genetic signature. Put another way, our DNA vaccines combat cancer by activating the body’s own immune system to identify and attack cancer cells.

Cytokine Therapy
〇 Interleukin-2 Gene
When introduced into immune cells, the product of this gene stimulates a subset of immune cells known as natural killer (NK) cells, which demonstrate natural cytotoxicity towards cancer cells.
〇 Interleukin-12 Gene
The product of this gene induces T cell- and NK cell-mediated immunity. It also prevents the generation of cancer cells.
〇 Interleukin-24 Gene
This tumor suppressor gene plays an important role in inducing selective apoptosis in human cancer cells and inhibits the growth of various types of cancer cells.
Natural Killer (NK) Cell Therapy
NK cell therapies are manufactured by isolating native NK cells from the blood of a patient, activating them to enhance their cytotoxicity, and then transfusing them back into the donor patient.





